
Massive transfusion protocol professional#
He has completed fellowship training in both intensive care medicine and emergency medicine, as well as post-graduate training in biochemistry, clinical toxicology, clinical epidemiology, and health professional education. He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives.Īfter finishing his medical degree at the University of Auckland, he continued post-graduate training in New Zealand as well as Australia’s Northern Territory, Perth and Melbourne. He is on the Board of Directors for the Intensive Care Foundation and is a First Part Examiner for the College of Intensive Care Medicine. He is also a Clinical Adjunct Associate Professor at Monash University. He is a co-founder of the Australia and New Zealand Clinician Educator Network (ANZCEN) and is the Lead for the ANZCEN Clinician Educator Incubator programme. Non-febrile haemolytic transfusion reactionĬhris is an Intensivist and ECMO specialist at the Alfred ICU in Melbourne.Acute / delayed haemolytic transfusion reaction.other problems including loss of identity, crossmatching issues, loss of baseline haematological information etc).risks of hurried cross-checking and incompatibility (allocation of sufficient resources and personnel, standard programs in place to facilitate process and anticipate needs).distractions resulting in not controlling source of haemorrhage, and.Difficulty with cross-matching future blood product.Haemolytic disease of newborn if RhD mismatch.disease transmission (use of products only on a needed basis only, standard blood banking precautions etc).hyperkalaemia (use of younger blood, monitor regularly, may require specific therapy).excessive citrate causing metabolic alkalosis and hypocalcaemia (monitor pH and ionised calcium, replace calcium as necessary).Transfusion related acute lung injury (consider use of filters, leukodepletion).
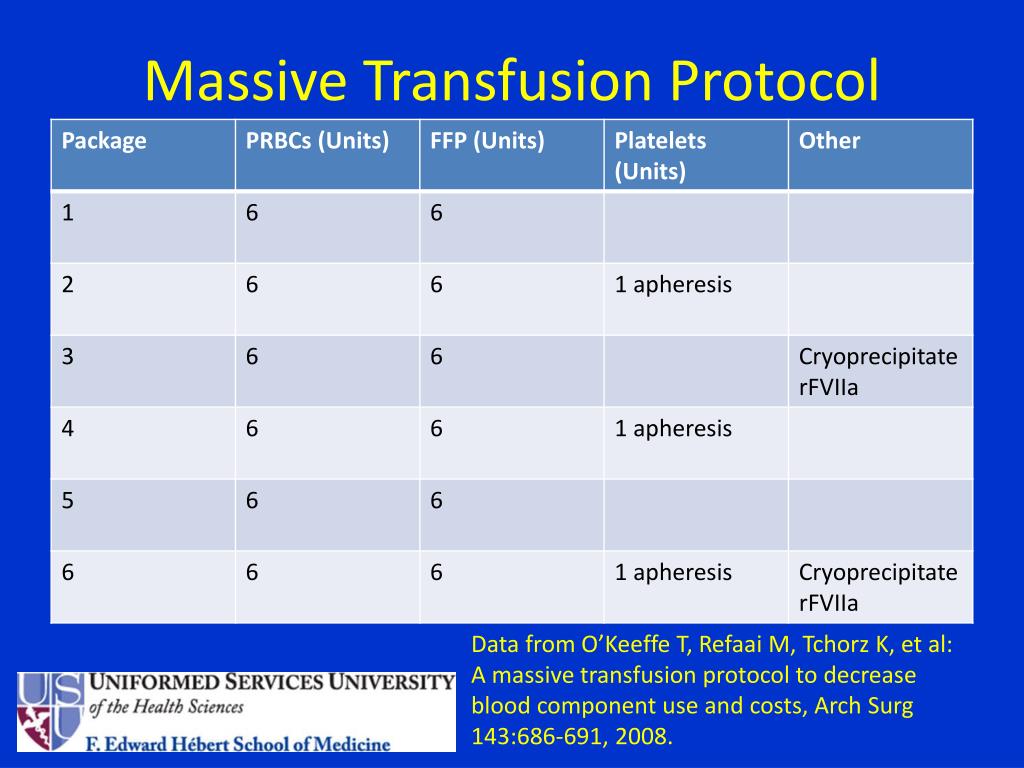

Risks and complications of large volume resuscitation with blood products See Massive transfusion protocol template.≥ 50 x 10^9 /L (>100 x 10^9 if head injury/ intracranial haemorrhage) This should not be used alone as transfusion trigger and, should be interpreted in context with haemodynamic status, organ & tissue perfusion.


 0 kommentar(er)
0 kommentar(er)
